As Parkinson’s progresses, we provide increasing levels of care for daily activities while helping seniors maintain their independence as much as possible.
Parkinson’s disease (PD) is a progressive neurodegenerative disorder that impacts millions of people around the world. It creates physical and cognitive challenges for the seniors diagnosed with it and also impacts their loved ones and caregivers. As certain nerve cells in the brain degenerate due to PD, seniors become deficient in dopamine and lose control of movement. This results in unwanted tremors, stiffness, slow movement, problems with balancing, and cognitive change.

Caregiver assistance can help seniors with PD navigate both physical and cognitive difficulties and improve their overall quality of life.
Family members and loved ones can also benefit from the role that caregivers play, as they no longer need to be alone in their efforts to provide support and excellent care. As Parkinson’s disease progresses, symptoms can become increasingly challenging to manage without a trained caregiver to help and provide relief. Fortunately, with their help, family members can find it much easier to prevent burnout, take breaks, and ensure their loved one is getting the care they deserve.
Here are just a few ways in which we support seniors with Parkinson’s:

Our caregiving team supports patient health by shopping, cooking, and serving nutritious foods that help fight against Parkinson’s. By focusing on highly nutritious foods, we help seniors build strength in their bones and muscles. A healthy, fiber-rich diet has many important benefits and can help prevent muscles from deteriorating, reduce the accumulation of body fat, and set seniors up for higher levels of health in the long run.
Neurodegenerative disorders like Parkinson’s can cause patients to experience tremors, shakes, and stiffness in their muscles. Our experts help patients with these symptoms by incorporating light activities such as walking and stretching. Rose’s caregivers make everyday activities easier by supporting patients as they carry out tasks and strive for independence in their daily lives.
People with Parkinson’s may need assistance in managing medications as their disease progresses. With multiple prescriptions, it can be difficult to keep track of the various medications that need to be taken on a regular basis. Thankfully, our caregivers are highly experienced in this area and help remind seniors to take their medication at the right time. Doing so helps ensure that seniors with Parkinson’s are functioning as well as possible.
Seniors with Parkinson’s can benefit greatly from our experienced personal care techniques. Depending on their needs, Rose’s caregivers help with everyday hygiene tasks such as taking a bath, getting dressed, and going to the bathroom. We help seniors plan ahead and establish beneficial routines while making sure to respect their privacy at all times.
It can be difficult for seniors with Parkinson’s to drive with the tremors and shakes they experience. Our caregiving team has years of experience in safely driving patients to doctor’s appointments, rehabilitation sessions, pharmacies, and more. We work hard to support our Parkinson’s patients with everyday errands while providing reliable transportation options.
Our trained caregivers know what it takes to lower the risk of falling for seniors with Parkinson’s. Exercise significantly reduces fall risk for seniors and can help those with Parkinson’s regain some of their balancing reflexes. Another area of focus for our caregivers is the home environment. To prevent falls from happening, they help make sure that tripping hazards are removed from the floor. It’s also important to tuck away any loose cables and ensure the floor is dry at all times.
It is common for seniors with Parkinson’s to experience different symptoms from day to day. When starting something new, such as therapy or medication, it’s important to note the impact on the individual’s overall well-being. Caregivers can be a big help when it comes to observing changes in symptoms, abilities, and moods over time. They understand the importance of being patient and flexible with seniors that may be frustrated, upset, or saddened by their situation.
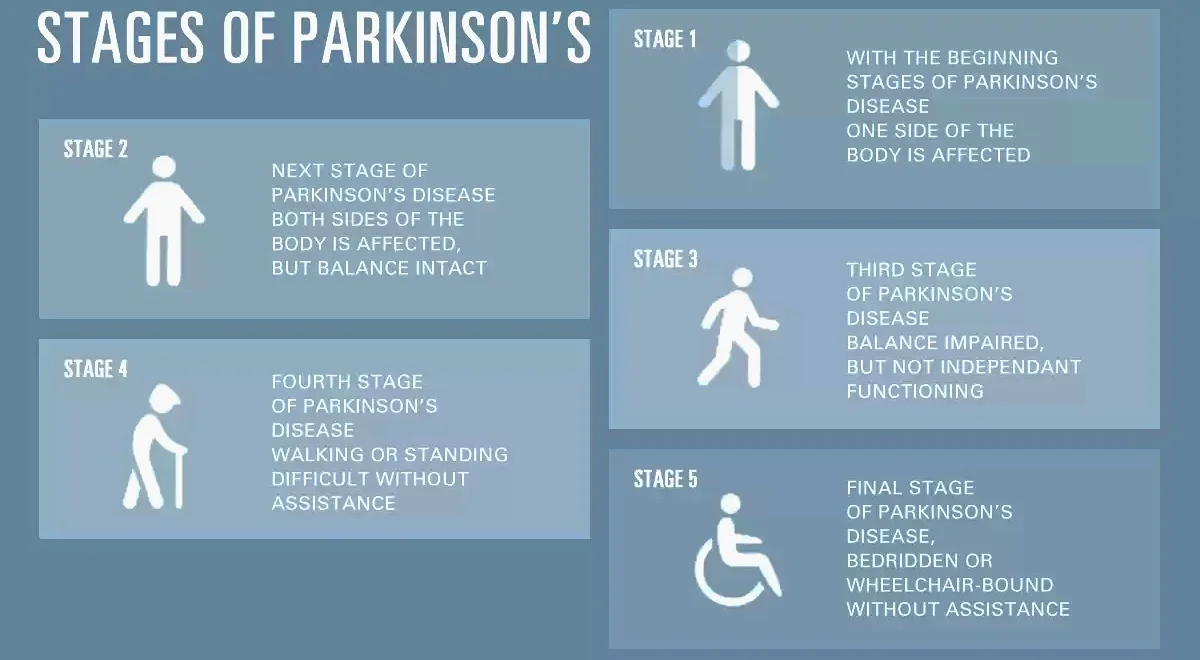
During this initial stage, the person has mild symptoms that generally do not interfere with daily activities. Tremor and other movement symptoms occur on one side of the body only. Changes in posture, walking and facial expressions occur.
Symptoms start getting worse. Tremor, rigidity and other movement symptoms affect both sides of the body or the midline (such as the neck and the trunk). Walking problems and poor posture may be apparent. The person is able to live alone, but daily tasks are more difficult and lengthier.
Considered mid-stage, loss of balance (such as unsteadiness as the person turns or when he/she is pushed from standing) is the hallmark. Falls are more common. Motor symptoms continue to worsen. Functionally the person is somewhat restricted in his/her daily activities now, but is still physically capable of leading an independent life. Disability is mild to moderate at this stage.
At this point, symptoms are fully developed and severely disabling. The person is still able to walk and stand without assistance, but may need to ambulate with a cane/walker for safety. The person needs significant help with activities of daily living and is unable to live alone.
This is the most advanced and debilitating stage. Stiffness in the legs may make it impossible to stand or walk. The person is bedridden or confined to a wheelchair unless aided. Around-the-clock care is required for all activities.
At its simplest, pain means the body hurts. When a person feels pain, nerves in the skin, joints and organs alert the brain to the location of an injury. Researchers have found that in early PD, there are already changes in the way that the body detects and regulates pain. Pain is complex and can take many forms. In PD, pain tends to affect the side of the body where motor symptoms first appeared. If your PD started with a tremor in the right hand, you’re more likely to develop pain in the right shoulder, wrist or fingers. Here are a few common types.
Musculoskeletal pain is experienced by up to 75 percent of people with PD and includes pain in the muscles, bones or skeleton. It is related to rigidity and decreased movement, and to arthritis. Many people with PD experience muscle cramps and tightness in the neck, spine and arms. Muscles may feel stiff or achy. Joint pain, especially in one shoulder, is also common. It’s not uncommon for people with PD to be diagnosed with frozen shoulder or rotator cuff problems, and even undergo surgery.
Do you have painful curling of your foot, toes or hands? This is dystonia, a painful muscle spasm. Up to 50 percent of people with PD experience this at some stage of the disease. Foot dystonia is one of the most common sources of dystonic pain in early PD. Severe, painful spasms also can occur in the neck, face or throat muscles. Dystonia may occur spontaneously or may be triggered by certain movements, but is very often experienced in the early morning. It can also be related to fluctuations in PD medications. Report dystonia to your doctor for evaluation or recommendations.
Also called radicular pain, neuropathic pain occurs when a nerve is crushed or inflamed. Between five and 30 percent of people with PD experience neuropathic pain. It feels sharp, electric, tingling or like coolness or numbness. In people with PD, changes in posture, as well as dystonia, can cause nerves to be crushed. A common type is sciatica - lower back pain that extends down one leg. People with PD may also experience peripheral neuropathy - injury to nerve endings that begins with numbness in the toes or fingertips.
Central pain affects about 10 percent of people with PD at some point. It can be difficult to describe but may include a vague, constant boring sensation; abdominal pain, reflux, shortness of breath or feeling flushed; painful sensations around the mouth, genital or rectal areas or simply “pain all over.”
It is critical to ensure your PD medications are working to their best ability. Your doctor may want to examine you immediately before and after you take PD medications. To increase, decrease or change your medication to extend its effectiveness.
Exercise is beneficial, particularly for musculoskeletal pain, but it can be a catch-22. It may be difficult to exercise when you’re in pain, but if you’re in pain and you stop moving, it gets worse! A physical therapist can recommend exercises or techniques to target the source of your pain. For example, if you experience neuropathic pain, the physical therapist can help improve your posture, which may alleviate pain.
Chronic pain and depression are intertwined. If a person experiences depression, it may worsen pain and other PD symptoms. In addition, people who are depressed have a hard time taking medications properly, and this sets a vicious cycle in motion: with missed doses, medications don’t work well, and a person feels worse. Treating depression is essential for managing pain. It’s also important to treat other health conditions, such as osteoporosis or diabetes, that impact pain.
If pain is long lasting (chronic), apply heat to the area for 15-20 minutes. Purchase a microwaveable hot pack that
conforms to the area (or make your own with rice in a tube sock knotted at the opening). Heat pack according to
directions; heat rice-filled sock for approximately two minutes in microwave.
If muscles feel tense or “knotted,” try self massage. Apply pressure to the area with a tennis ball, using your
body weight against it for deeper pressure. Knobby plastic massage tools or a Theracane can be used to get better
leverage on hard-to-reach areas. An appointment with a massage therapist may also be helpful.
"I can't think RAHC enough for the support they provided my mother during her time of greatest need. Despite her changing care requirements and her daily (even hourly) fluctuations in the hours she needed, they always managed to stay on top of it."
"Rose's Agency Home Care has helped with everything from clothing, to cleaning, to washing, and medication. Rose's Agency Home Care just cares. They're really professional. They always know exactly what to do and what to expect from the patient."
"I appreciated their helpfulness and their willingness to work with us on the price, we have loved the two caregivers they sent us. My grandmother has been particularly difficult to please and I am happy to report that I found an agency that was able to satisfy her."